What's in a name?
By Alan Hickey
As we are in the middle of Idiopathic Hypersomnia Awareness Week and are heading towards World Narcolepsy Day, Sept. 22, it is a good time to take reflect on the current thinking of these primary sleep disorders. By primary, I mean they are not caused by another illness. They stand on their own two feet as a real disorder.
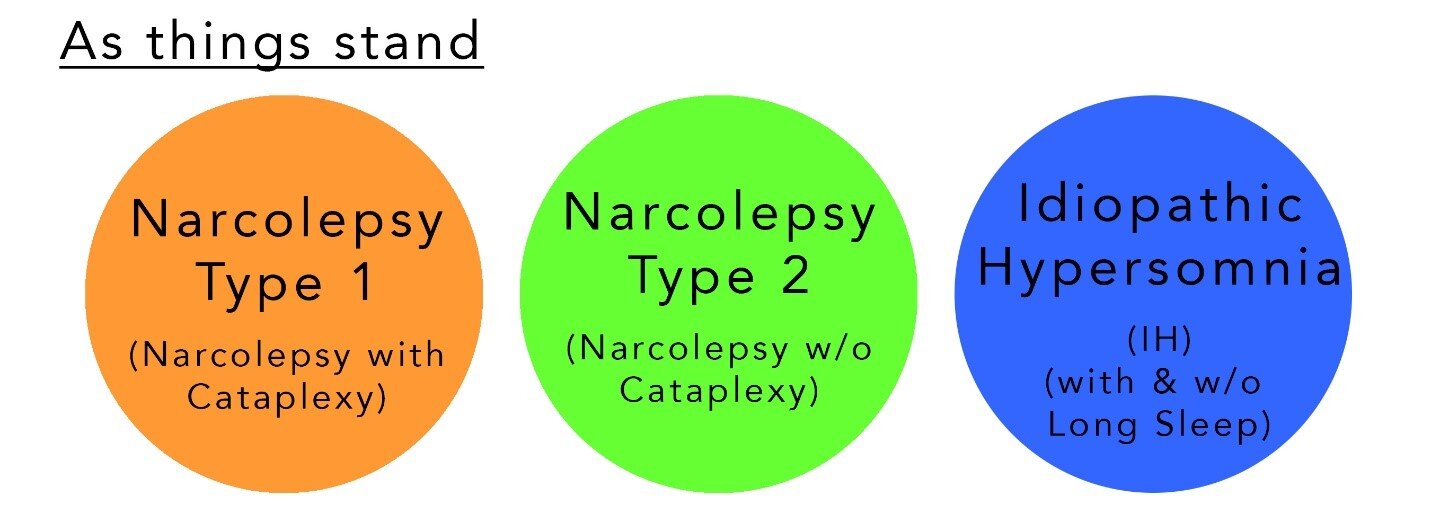
Sleep disorders are described and essentially set in stone in the International Classification of Sleep Disorders (ICSD). The last time that they have been updated was back in 2014. Since then there has been a lot of science conducted. Admittedly, due to financial limitations that research has mainly focused on narcolepsy type 1 (NT1/narcolepsy with cataplexy) because there already existed a good foundation to expand on and, quite frankly, the experience of NT1 in patients was more clear cut which is extremely important when you want to evaluate if a treatment is working or not.
In 2014, there was a move away from narcolepsy with and without cataplexy labels to narcolepsy type 1 and 2.
If you are reading this, I am going to assume you already know about these classifications and how the medical field distinguishes between them. In August 2020, a paper was published in Sleep Medicine Reviews and can be found at this link (https://doi.org/10.1016/j.smrv.2020.101306).
In this paper, Lammers et al highlight that the above classifications are six years old and are in need of updating to reflect the current scientific understanding of the neurological mechanisms of the disorders. The authors propose new guidelines with the aim of starting a discussion on how to update the diagnostic criteria which determines which sleep disorder best matches the patient’s symptoms.
By neurological mechanism of the sleep disorders they are talking about genetic biomarkers. The HLA typing biomarker DQB1∗06:02 has been identified as key factor in whether someone with one of these sleep disorders will develop cataplexy. While DQB1∗06:02 is common in the general population (in other words, having it does not mean you will develop cataplexy), it is found in 98% of people with NT1.
As we know, some people with NT2 can develop cataplexy at a later date and again those individuals typically have the DQB1∗06:02 biomarker.
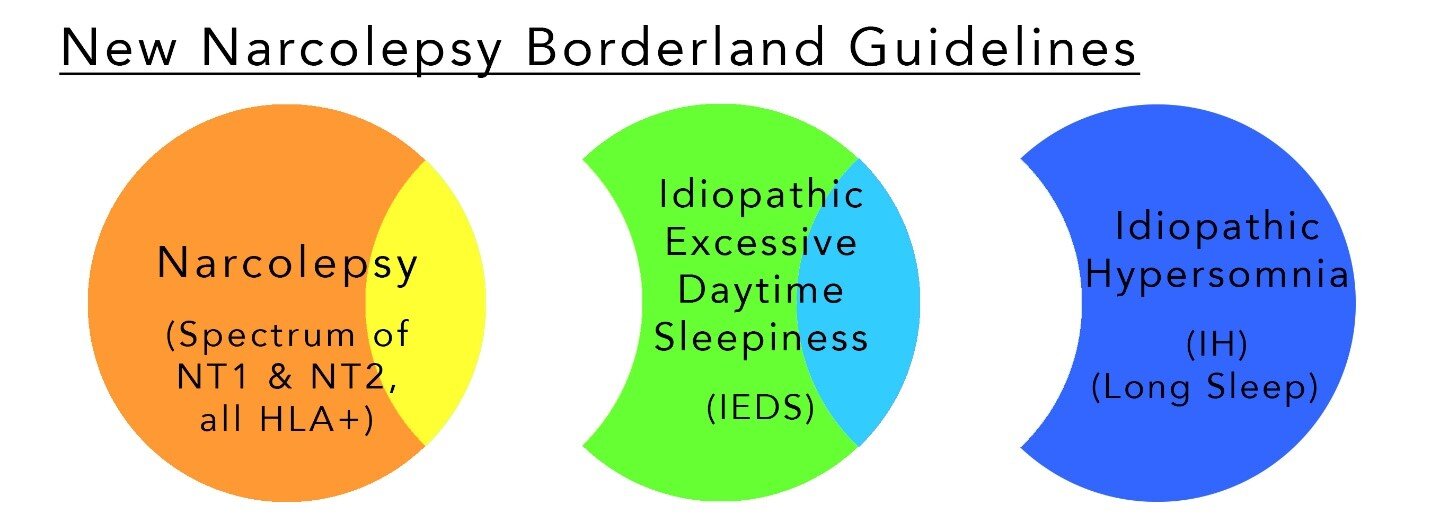
Based on that finding, (in simple terms) the new guidelines suggest that narcolepsy is a spectrum disorder consisting of the NT1 group and those in the NT2 group who have the DQB1∗06:02 biomarker.
Less well known is the fact that the polysomnography (PSG or sleep study) and the multiple sleep latency test (MSLT) results are not very reproducible in NT2 and IH patients. Depending on the study, the individual can be classified as one or the other and move between the disorders with each study.
This is a major shortcoming of the current classifications. In some countries, it also affects what medicine is covered by insurance companies to treat the symptoms.
In the idiopathic hypersomnia classification, there are two main groupings – with and without the need for long sleep time which is defined as sleeping 10 or more hours a day.
The new guidelines suggest separating those two IH groups. If adopted, IH would become a classification for people with excessive need for sleep (ENS) – those with long sleep time.
The remaining NT2 patients and the IH patients without the need for a long sleep time would then be combined creating a new classification – idiopathic excessive daytime sleepiness (IEDS).
In effect, the new proposals eliminate the ‘with or without cataplexy’ designations, combining them into simply narcolepsy. So, no more NT1 and NT2.
It creates a new category – idiopathic excessive daytime sleepiness (IEDS) that is made up of the people with narcolepsy without cataplexy that don’t have the HLA typing biomarker and the people with idiopathic hypersomnia that do not have long sleep time. They also propose subtypes within this category: REM Type, NREM (non-REM) Type and Attention Type.
Finally, the people with idiopathic hypersomnia and long time will be known as simply idiopathic hypersomnia, if these guidelines are adopted as is.
There are a lot more details on the criteria for each category and subtypes in the published paper (https://doi.org/10.1016/j.smrv.2020.101306). This is just a brief introduction that has the same goal as the paper itself – to get a discussion started.
One benefit of the proposals/paper, is the acknowledgement that the research needs to shift from understanding the neurological mechanism of NT1 to idiopathic excessive daytime sleepiness and idiopathic hypersomnia.
What do you think about the new guidelines? How will they affect you?